Introduction
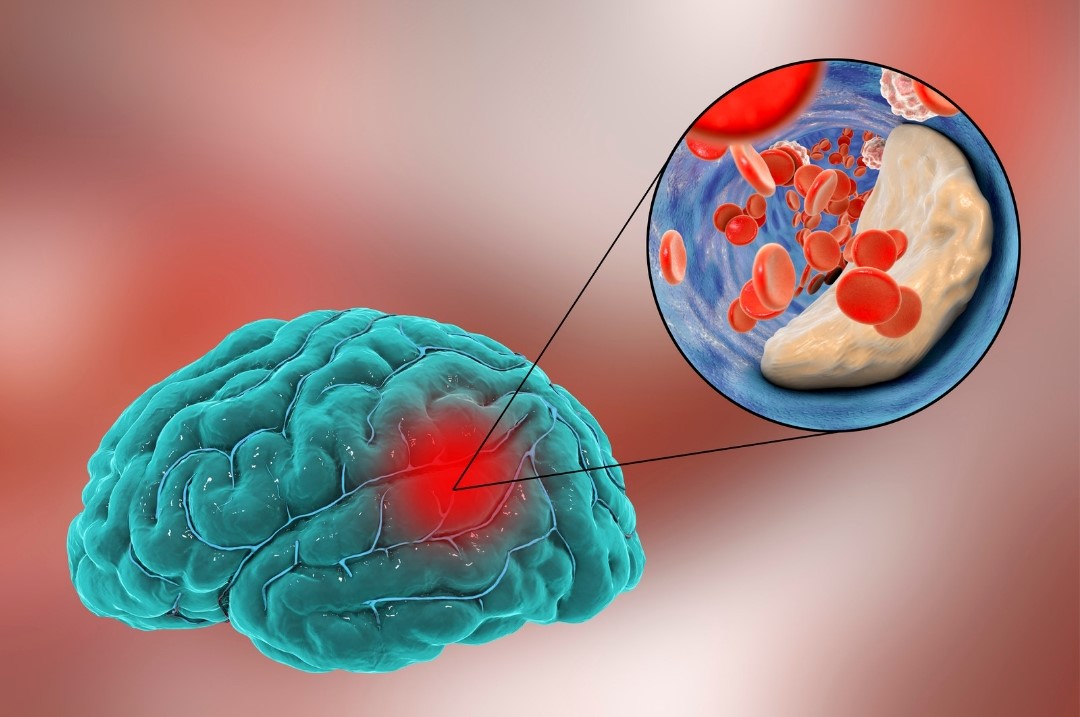
Ischemic stroke, a leading cause of disability and death worldwide, occurs when a blood clot obstructs the flow of blood to the brain, leading to brain cell death1. Prompt treatment is crucial to minimize damage and improve outcomes. Two primary interventions for ischemic stroke are Tissue Plasminogen Activator (TPA) and mechanical thrombectomy2.
Understanding Ischemic Stroke
Ischemic strokes account for approximately 87% of all stroke cases3. The leading cause is the blockage of cerebral arteries, which can occur due to various factors, such as:
- Atherosclerosis (plaque build-up)
- Atrial fibrillation
- Other cardiovascular conditions
Recognizing the symptoms of a stroke is essential for timely intervention. Symptoms may include:
- Sudden numbness or weakness in the face, arm, or leg, particularly on one side of the body
- Confusion, trouble speaking, or understanding speech
- Difficulty seeing in one or both eyes
- Trouble walking, dizziness, or loss of balance and coordination
TPA: The Clot-Busting Drug
Tissue Plasminogen Activator (TPA) is a medication that dissolves blood clots in ischemic stroke patients [4]. Administered intravenously, TPA converts plasminogen to plasmin, which breaks down the clot. The use of TPA is time-sensitive, typically effective within 3 to 4.5 hours from the onset of symptoms4.
Advantages of TPA
- Non-invasive: Administered through an IV.
- Quick action: This can quickly dissolve the clot if administered promptly.
Limitations of TPA
- Time constraint: Must be given within a narrow time window.
- Risk of haemorrhage: This can increase the risk of bleeding, including intracranial haemorrhage.
- Deranged PT(>15 seconds) and INR(>1.7) is a contraindication for TPA.
Mechanical Thrombectomy: The Direct Approach
Mechanical thrombectomy is a minimally invasive surgical procedure that physically removes the clot from the artery. This technique is especially effective for large vessel occlusions and can be performed even after the TPA window has closed, up to 24 hours in some5.
Advantages of Mechanical Thrombectomy
- Effective for large vessel occlusions where TPA may be less effective.
- Extended time window for treatment.
- Can be used in conjunction with TPA for a better outcome.
Limitations of Mechanical Thrombectomy
- Requires specialized equipment and expertise.
- Invasive procedure: Involves threading a catheter through the arteries to the brain.
- Availability: Not all hospitals are equipped to perform this procedure.
TPA vs. Mechanical Thrombectomy: Which is Better?
Both TPA and mechanical thrombectomy play crucial roles in the management of ischemic stroke. The choice between the two depends on various factors, including:
- Time of Onset: TPA is preferred within the initial 4.5 hours, while thrombectomy is viable for up to 24 hours.
- Location and Clot Size: Thrombectomy is more effective for large vessel occlusions.
- Patient’s Health and Contraindications: TPA may be contraindicated in patients with a high risk of bleeding.
Combined Treatment Approach
In some cases, a combined approach is used where TPA is administered first to dissolve the clot, followed by mechanical thrombectomy if the clot persists. This approach has shown promising results in improving patient outcomes, particularly in cases of large vessel occlusion.
Conclusion
The treatment of ischemic stroke has advanced significantly with the advent of TPA and mechanical thrombectomy. While TPA offers a quick, non-invasive option, mechanical thrombectomy provides an effective solution for cases where TPA may not suffice. The decision between TPA and mechanical thrombectomy should be made based on the specific circumstances of each patient to minimize brain damage and improve recovery.
FAQs
What is TPA, and how does it work?
TPA is a clot-dissolving drug used in ischemic stroke to break down blood clots and restore blood flow to the brain.
When is mechanical thrombectomy recommended?
Mechanical thrombectomy is recommended for patients with large vessel occlusion, mainly when the clot cannot be effectively treated with TPA alone.
Can TPA and mechanical thrombectomy be used together?
Yes, in some cases, both treatments are combined to enhance the chances of a successful outcome.
What are the risks of TPA?
The primary risk of TPA is the increased likelihood of bleeding, including potentially life-threatening intracranial haemorrhage.
Is mechanical thrombectomy available at all hospitals?
Mechanical thrombectomy requires specialized equipment and expertise; not all hospitals can perform the procedure.
Footnotes
- Tuo, Q.z., S.t. Zhang, and P.J.M.r.r. Lei, Mechanisms of neuronal cell death in ischemic stroke and their therapeutic implications. 2022. 42(1): p. 259-305. ↩︎
- Fischer, U., et al., Primary thrombectomy in tPA (tissue-type plasminogen activator) eligible stroke patients with proximal intracranial occlusions. 2018. 49(1): p. 265-269 ↩︎
- Béjot, Y., B. Daubail, and M.J.R.n. Giroud, Epidemiology of stroke and transient ischemic attacks: Current knowledge and perspectives. 2016. 172(1): p. 59-68. ↩︎
- Liu, S., et al., Tissue plasminogen activator-based nanothrombolysis for ischemic stroke. 2018. 15(2): p. 173-184. ↩︎
- Katz, J.M., et al., Mechanical embolectomy. 2005. 16(3): p. 463-474. ↩︎
- Tuo, Q.z., S.t. Zhang, and P.J.M.r.r. Lei, Mechanisms of neuronal cell death in ischemic stroke and their therapeutic implications. 2022. 42(1): p. 259-305.
- Fischer, U., et al., Primary thrombectomy in tPA (tissue-type plasminogen activator) eligible stroke patients with proximal intracranial occlusions. 2018. 49(1): p. 265-269
- Béjot, Y., B. Daubail, and M.J.R.n. Giroud, Epidemiology of stroke and transient ischemic attacks: Current knowledge and perspectives. 2016. 172(1): p. 59-68.
- Liu, S., et al., Tissue plasminogen activator-based nanothrombolysis for ischemic stroke. 2018. 15(2): p. 173-184.
- Katz, J.M., et al., Mechanical embolectomy. 2005. 16(3): p. 463-474.