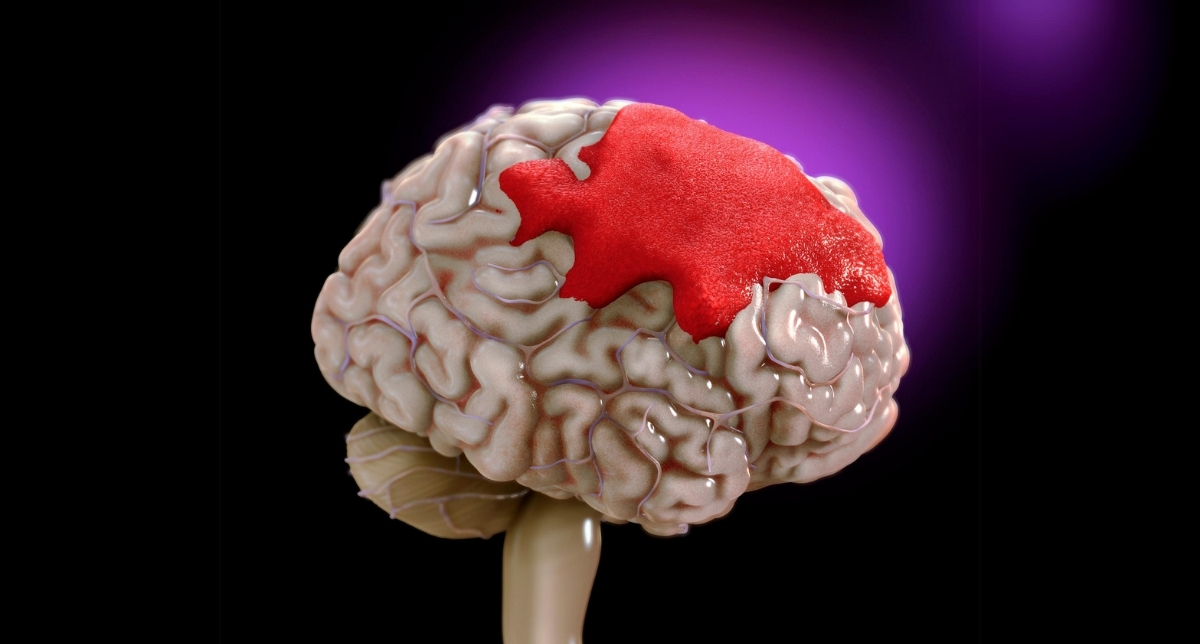
In the medical world, intracranial hemorrhage is considered a serious medical condition due to bleeding within the skull. Nevertheless, most cases of intracranial hemorrhage have severe neurological consequences when not appropriately treated promptly.
The knowledge of what causes, types, symptoms, diagnoses, and treatments exist for intracranial hemorrhage can provide useful information on preventive measures and treatment.
What is Intracranial Hemorrhage?
Bleeding from blood vessels within the skull to lead to an accumulation of blood within or around the brain is known as intracranial hemorrhage. The build-up raises intracranial pressure and compresses the tissues often interfering with normal brain activities. It’s also taken to be a medical emergency that usually calls for prompt intervention to minimize as much damage to the brain as possible and enhance chances of recovery.
Types of Intracranial Hemorrhage
There are different types of intracranial hemorrhage and each differs in its location of bleed:
Epidural Hemorrhage (EDH):
- Situated between the dura mater (outer brain membrane) and the skull.
- Commonly linked with a head injury, leading to a transient loss of consciousness that may be punctuated by a period of apparent recovery or lucidity, followed by deterioration.
Subdural Hemorrhage (SDH):
- It lies between the dura mater and the arachnoid membrane.
- Commonly caused by trauma, but can also occur spontaneously in the elderly or anticoagulated patients
Subarachnoid Hemorrhage (SAH):
- There is bleeding between the arachnoid and pia mater.
- Usually, a ruptured aneurysm causes SAH, leading to a sudden, severe headache known as a “thunderclap” headache.
Intracerebral Hemorrhage (ICH):
- The bleeding occurs within the brain tissue itself.
- Can result from hypertensive cause, trauma, or other vascular malformation.
Intraventricular Hemorrhage (IVH):
- Bleeding into the brain’s ventricular system, where cerebrospinal fluid is produced.
- Often seen in premature infants but may occur in adults with severe trauma or other brain conditions.
Causes and Risk Factors
Intracranial hemorrhage can result from several causes; the following are the most common:
- Trauma: This is a common cause of epidural and subdural hemorrhages.
- Hypertension: Prolonged elevated blood pressure can damage vessels, which therefore results in intracerebral hemorrhage.
- Aneurysms and Arteriovenous Malformations (AVMs): Vessels become abnormally developed in the brain, and may burst.
- Blood Clotting Disorders: These include conditions like hemophilia as well as drugs like anticoagulants, that may cause an increased risk for bleeding.
- Tumors: Some types of brain tumors may cause or predispose a patient to hemorrhage.
- Lifestyle factors: Smoking, excessive alcohol intake, and recreational drug abuse, such as cocaine and amphetamines, cause vascular damage.
Symptoms of Intracranial Hemorrhage
The symptoms of intracranial hemorrhage depend on the size, location, and speed of the bleeding. Some of the common signs and symptoms are as follows:
- Sudden severe headache: It is often described as the “worst headache of my life”; it is more typical of SAH.
- Nausea and vomiting: Due to increased intracranial pressure.
- Confusion or altered mental status: It varies from slight confusion to coma.
- Weakness or paralysis: Generally, one-sided and most commonly unilateral limb weakness.
- Vision changes: loss of vision, double vision, or blurred vision.
- Inability to communicate with others: Unable to speak or not able to understand people.
- Seizures: Especially so in hemorrhages resulting in cerebral cortex damage.
Diagnosing Intracranial Hemorrhage
Prompt diagnosis is crucial to the effective management of intracranial hemorrhage. The common diagnostic tools in use include the following:
- CT-Scan: The most common diagnostic tool for making a distinction regarding the nature and extent of the hemorrhage. In CT scans, blood in the brain is sufficiently rendered so that all necessary information can be used to initiate the appropriate treatment.
- MRI (Magnetic Resonance Imaging): It offers more detail than with CT scanning, especially on smaller hemorrhages or slight changes in the brain.
- Angiography: This is given for vascular visualization and defining the source of bleeding, for example, aneurysms or AVMs.
- Lumbar Puncture: If subarachnoid hemorrhage is suspected, but imaging is inconclusive, then a lumbar puncture might be used to confirm this condition since elevated blood in cerebrospinal fluid can confirm this.
Treatment Options for Intracranial Hemorrhage
The management for intracranial hemorrhage is decided on the causes, type, and location of bleeding. Besides all these, the general health condition of the patient also has to be considered.
Surgical Treatments:
- No Craniotomy: An Open Procedure: It is a kind of open surgery which involves the removal of the clot from the brain to drain off the pressure.
- Stereotactic Aspiration: It is less invasive than a craniotomy. Here imaging technique guides the clinician on how to insert the needle at the site of hemorrhage for clot removal.
- Endovascular Procedures: Coiling or embolization of aneurysms or AVMs prevents further bleeding.
Medication Management:
- Blood Pressure Management: Administered antihypertensive drugs lower the risk of re-bleeding.
- Anticoagulation Reversal: If blood-thinning drugs cause the bleeding, certain agents could be utilized to reverse their effects.
- Anti-Seizure Medications: Administered either as a preventive measure or for treatment of seizures.
- Osmotic Agents: Mannitol and the like draw fluid from the brain tissue to reduce intracranial pressure
Supportive Care:
- ICU Monitoring: Patients with intracranial hemorrhage are often put on very close monitoring in the ICU for the assessment of neurological function and prevention of complications.
- Physical and Speech Therapy: Most patients require rehabilitation after stabilization due to lost functions depending on the degree and location of the hemorrhage.
Prevention of Intracranial Hemorrhage
Whereas all the possible causes of intracranial hemorrhage cannot be prevented, certain measures that are evitable can reduce the risk to a certain extent:
- Management of Hypertension: General management of high blood pressure can prevent spontaneous intracerebral hemorrhage.
- Abstinence from Smoking and Excessive Alcohol Consumption: Both can enhance the chance of vascular illness.
- Monitoring in At-Risk Persons: The individual who has an aneurysm, AVM, or a coagulation disorder should be more careful about follow-up through health care.
- Protective Measures in High-Impact Activities: The wearing of helmets, seat belts, and other gear where high risks of head injury are involved while participating in such activities.
- The advent of Medication: Patients on anticoagulants should be carefully monitored and counselled on possible risks of bleeding.
Prognosis and Outcomes
The outcome of intracranial hemorrhage patients is highly variable. The prognosis depends on the location, size of the hemorrhage, age of the patient, and their overall medical condition, among other factors. Additionally, the time to treatment influences outcomes. In general:
- Epidural Hemorrhage: It may have a good prognosis if treated in time; however, most such cases are fatal without medical care.
- Subdural Hemorrhage: It depends upon the amount of bleeding present in a patient and the patient’s age; chronic cases may only require monitoring and acute cases normally require surgery.
- Intracerebral and Subarachnoid Hemorrhage: These have a higher mortality and disability rate with intracerebral hemorrhage being critical when it involves the brain regions.
Most patients after treatment rely on rehabilitation to regain all functions, such as motor, speech, and cognition. Thus, a multidisciplinary team including neurologists, physical therapists, and psychologists will help achieve maximum recovery and quality of life.
Conclusion
Intra cranial hemorrhage is among the most serious conditions that are normally life-threatening; it calls for prompt medical care. Advances in medical imaging and surgical techniques have improved the outcome of patients suffering from intracranial hemorrhage; however, prevention through lifestyle adjustments and medical management of other underlying risk factors remains the best approach. Education and awareness can reduce the impact of this complex medical emergency.
References
- Caceres, J.A. and Goldstein, J.N., 2012. Intracranial hemorrhage. Emergency medicine clinics of North America, 30(3), pp.771-794.
- Huisman, T.A., 2005. Intracranial hemorrhage: ultrasound, CT and MRI findings. European radiology, 15(3), pp.434-440.
- Mandybur, T.I., 1977. Intracranial hemorrhage caused by metastatic tumors. Neurology, 27(7), pp.650-650.
- Naidech, A.M., 2011. Intracranial hemorrhage. American journal of respiratory and critical care medicine, 184(9), pp.998-1006.
- Parizel, P., Makkat, S., Van Miert, E., Van Goethem, J., Van den Hauwe, L. and De Schepper, A., 2001. Intracranial hemorrhage: principles of CT and MRI interpretation. European radiology, 11, pp.1770-1783.
- Tenny, S. and Thorell, W., 2017. Intracranial hemorrhage.