Introduction
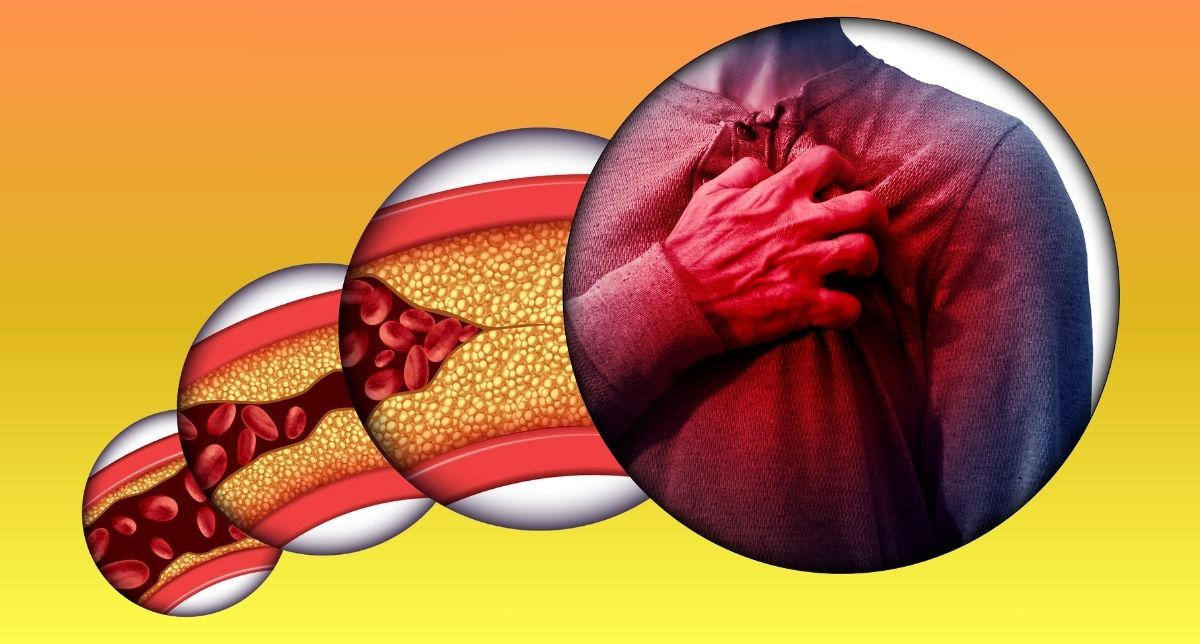
Acute coronary syndrome is a spectrum of urgent cardiac diseases that include unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI). Rapid recognition and treatment in an emergency situation are of the utmost importance for improved patient outcomes and the elimination of complications that, for instance, such a condition might cause heart failure or lead to death.
1. Initial Assessment
THE INITIAL STEP IN THE MANAGEMENT OF ACS IS EARLY DIAGNOSIS. Which means a prompt ECG and sending relevant labs such as Trops, CKMB. Patients usually present with chest pain (typically pressure or tightness), shortness of breath, diaphoresis, nausea, or pain radiation to the jaw, shoulder, or arm. Sometimes, though, the patient will only complain of mild chest pain, with no apparent cause; they often have an impending sense of doom.
2. Immediate Measures
If ACS is suspected, the following measures should be initiated:
– Oxygen Therapy: Keep the patient on oxygen if saturation is <90%.
– Aspirin: 300 mg
– Clopidogrel 300mg
– Inj Enoxaparin 1mg/kg SC or Inj Heparin 1cc IV
– Nitroglycerin: Sublingual nitroglycerin (0.3–0.6 mg) can relieve chest pain if not contraindicated by hypotension.
Pain Control: Consider the use of morphine for unrelieved chest pain. If employed, it should be done so with extreme caution.
3. Diagnosis confirmation requires timely investigations:
– Electrocardiogram (ECG): Within 10 minutes of arrival, perform ECG to differentiate between STEMI/ NSTEMI/Unstable Angina.
– STEMI: ST-segment elevation myocardial infarction. It implicates complete coronary artery occlusion; management has to be immediate.
– NSTEMI/Unstable Angina: No ST elevation in them; but often there are T-wave changes or ST depression.
Cardiac Biomarkers: Confirmation of myocardial injury in cases of NSTEMI or STEMI is based on the troponin levels observed.
4. Management of STEMI
For cases confirmed as STEMI:
-Reperfusion Therapy: Time is critical—PCI should have a door-to-balloon time of fewer than 90 minutes or, in the absence of PCI, a door-to-needle time of fewer than 30 minutes.
-Antiplatelet Therapy: It should be initiated that includes dual antiplatelet therapy (for example aspirin + clopidogrel).
Anticoagulation: Start heparin or low molecular weight heparin.
5. NSTEMI/Unstable Angina Management
Patients with NSTEMI or unstable angina benefit from a tailored approach:
– Risk Stratification: Use tools like the GRACE or TIMI score to assess risk and guide invasive vs. conservative strategies.
– Medical Therapy: Initiate dual antiplatelet therapy, beta-blockers, and anticoagulation. Consider statins for lipid stabilization.
– Angiography: In high-risk patients, coronary angiography within 24–72 hours is advised.
6. Supportive Care
Throughout the management of ACS, supportive measures play a vital role:
– Continuous Monitoring: Place patients on cardiac monitors to detect arrhythmias or other complications.
– Communication: Regularly update patients and their families on the progress and next steps.
– Psychological Support: Address anxiety and stress, as these can exacerbate the condition.
7. Post-ACS Care
After stabilization, patients require long-term care to prevent recurrence.
– Medication Adherence: Reinforce the importance of antiplatelets, statins, ACE inhibitors, and beta-blockers.
– Lifestyle Modifications: Counsel on quitting smoking, adopting a heart-healthy diet, and maintaining regular physical activity.
– Follow-Up: Schedule timely cardiology consultations to monitor progress and adjust treatment plans.
Conclusion
Managing ACS in the emergency setting demands rapid assessment, timely interventions, and coordinated teamwork. By following the established protocols and maintaining a patient-centered approach, healthcare providers can significantly reduce mortality and enhance the quality of life for those affected by this critical condition.